Revolutionizing Ear Reconstruction: One Scar, Big Results
By Ha H. Nguyen, Huyen T. T. Tran, and Hang T. T. Nguyen
Department of Maxillofacial - Plastic - Aesthetic Surgery, Viet-Duc University Hospital, Hanoi, Vietnam
A Single Cut That Changes Lives
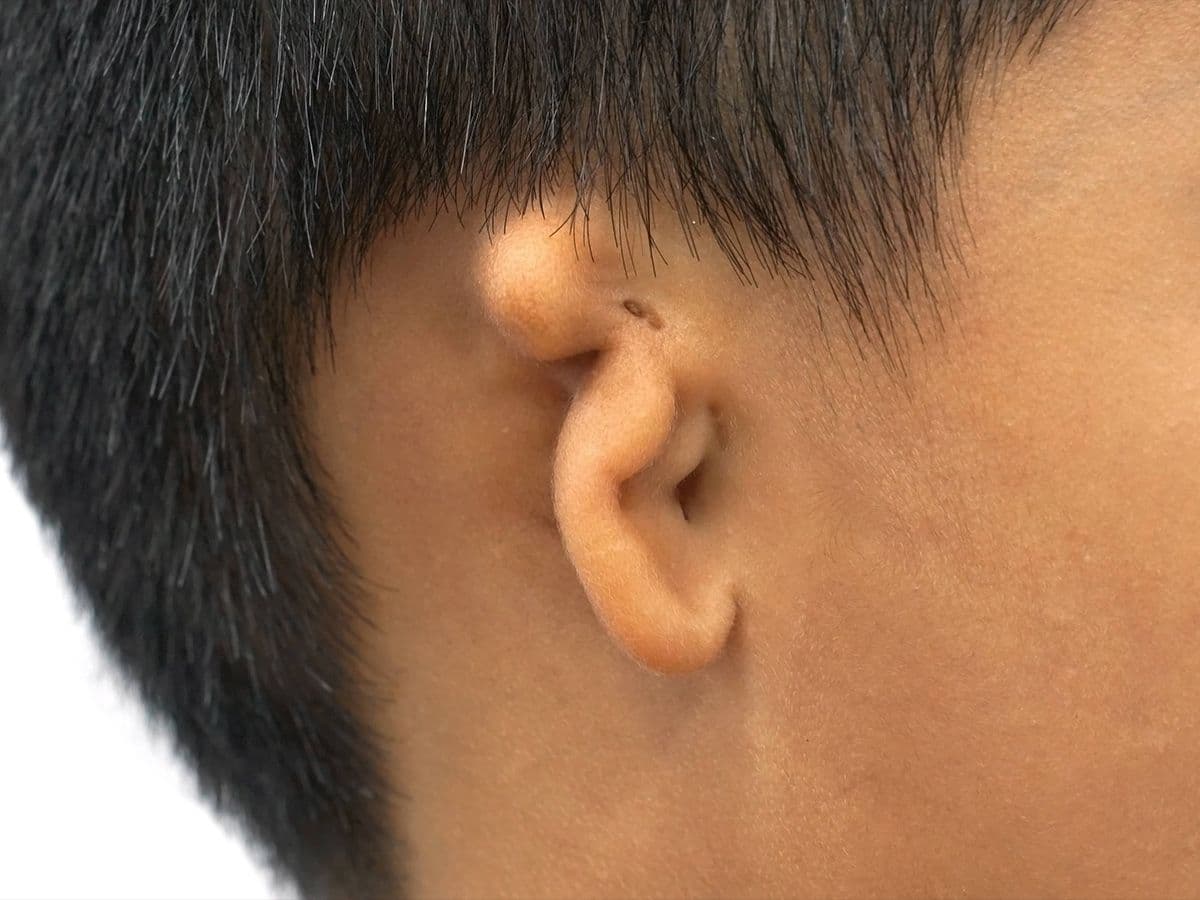
In the evolving field of reconstructive surgery, cosmetic outcomes matter just as much as functional success—especially for procedures that impact visible areas like the ear. Traditional auricular reconstruction techniques, while effective, often leave behind long scars and areas of hair loss. But what if we told you there's now a minimally invasive alternative?
Welcome to the era of single-incision, endoscopic-assisted temporoparietal fascia flap (TPFF) harvesting—a breakthrough that blends surgical precision with aesthetic sensibility.
The Challenge of Auricular Reconstruction
Auricular reconstruction for conditions like congenital microtia or trauma-related ear loss has long relied on two primary methods: autologous costal cartilage or porous polyethylene (PPE) frameworks. The cartilage option demands multiple stages and is delayed until children reach ages 8–12. PPE frameworks, introduced for younger children by Reinisch in the 1990s, allow earlier intervention but require meticulous soft tissue coverage to avoid complications like framework exposure.
Enter the TPFF—an ideal thin and vascular flap used to cover the ear framework. Historically, harvesting this flap meant long, conspicuous scalp incisions that often led to scarring and alopecia. Not anymore.
The Breakthrough Approach
From 2018 to 2021, our team at Viet-Duc University Hospital treated 60 patients using a novel single-incision technique. We used an endoscope and a single discreet incision hidden along the hairline to harvest TPFFs—entirely avoiding scalp scars.
Our key achievements:
- 61 flaps harvested with no flap necrosis or severe complications.
- Only 11.5% had minor framework exposures, all managed conservatively.
- One instance of facial nerve injury across all cases.
- Viable flaps with excellent blood supply, confirmed postoperatively.
We successfully reconstructed ears in patients ranging from 3 to 50 years old, with many young children receiving life-changing surgery before even starting school.
Why It Works
Using a 30° endoscope, we navigated the complex anatomy of the scalp with precision. We carefully preserved vital arteries such as the superficial temporal artery and its branches, ensuring flap viability. In some cases, we even identified additional small arteries previously undetectable by Doppler or CT angiography.
This method not only avoids unsightly scars but also reduces intraoperative blood loss, postoperative pain, and recovery time. Surgeons benefit from ergonomic ease and a magnified surgical field, and teaching this technique becomes easier via live video feed.
Looking Ahead
With this technique, we achieved both reconstructive goals and cosmetic excellence. And with 61 flaps—the largest series of its kind—we’re confident this approach can become the new gold standard for auricular reconstruction.
Our heartfelt thanks go to Dr. John Reinisch and Dr. Ken Stewart, pioneers in microtia reconstruction, for their guidance and inspiration.
For Patients and Parents
If you're a parent of a child with microtia or someone dealing with an ear defect, know that solutions are becoming not just better—but also more beautiful.